Listen to S5E2: Webinar highlights from The Overcoming MS Handbook: Roadmap to Good Health
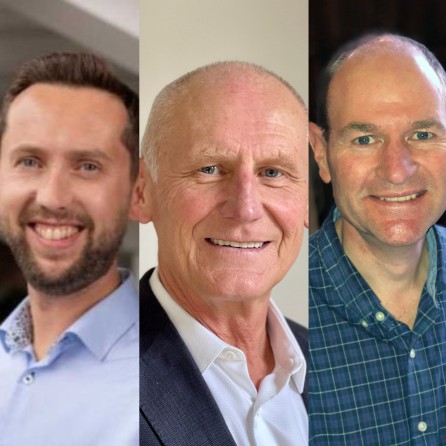
Welcome to Living Well with MS, the Overcoming MS podcast where we explore all topics relating to living well with multiple sclerosis (MS). In this episode, we are taking you back to the launch of the ‘Overcoming MS Handbook: Roadmap to Good Health’ with Professor George Jelinek, Dr Jonathan White and Dr Phil Startin. Together they discussed how the new book was created, the highlights from the book and answered questions from the community. We were excited by the arrival of the new book, as it provides an engaging overview of the Overcoming MS Program combined with stories from the community.
This webinar was recorded in February 2022 as part of our Finding Hope with Overcoming MS webinar series. You can watch the whole webinar here or the podcast highlights on YouTube here.
Keep reading for the key episode takeaways and George, Jonathan and Phil’s bios.
Professor George Jelinek said: “After what seems like quite a long time of bringing this message to people, I’m hearing the message come back to me through the filter of all of these different people’s lives and experiences, joys and sorrows. It’s just a wonderful read for me to sit down and say that all this has been happening in our community and that people have worked out ways of adopting and maintaining this program, many of which I’ve really never considered given that I’ve got only my own particular view of the world.”
Dr Jonathan White said: “I think sometimes the medical community thinks it’s “us or them” [with] lifestyle or medication and that could never be further from the truth. I personally have always chosen to use medication as part of my way of managing MS and I wouldn’t change that. But nor would I change using lifestyle to manage my MS. Undoubtedly for many people medication has many benefits and is a huge part of your armor and protection against this disease. But why ignore the underlying things that caused the problem in the first place, you know, stress, lack of exercise, low vitamin D levels, poor diet and processed and altered fats and animal fats in your diet?”
Dr Phil Startin said: “By following the Overcoming MS program, you absolutely can make a difference [to your MS], you can change the trajectory of that condition, and you can improve your quality of life. Through neuroplasticity, you can even recover some functions. The Overcoming MS program is just as relevant for us with a progressive form of the condition as it is for those with those newly diagnosed and with a relapsing form, possibly even more.”
Intro 00:04
Welcome to Living well with MS. This podcast comes to you from Overcoming MS. The world’s leading multiple sclerosis healthy lifestyle charity, which helps people live a full and healthy life through the Overcoming MS program. We interview a range of experts and people with multiple sclerosis. Please remember, all opinions expressed are their own. If you enjoy the show, please leave a review. These are quick to do and really help us. Today’s episode features highlights from the Overcoming MS Handbook: Roadmap to Good Health Webinar, presented by Professor George Jelinek, Dr. Jonathan white, and Dr. Phil starting and recorded live in front of our global audience as part of the Finding Hope with OMS series. To join us live for the next webinar, or to watch the original presentation, head to our website, overcomingms.org.
George Jelinek 01:00
And on behalf of the three of us, welcome to all of you who are listening in and watching tonight, and this morning, depending on where you are in the world, it’s just lovely to connect with a lot of people who I obviously know quite well, and I’m sure there’s plenty of newcommers too. I just wanted to start by telling you a little bit about the book and the what really is different about it, what was the inspiration behind producing it, how it differs from the previous OMS book. And I guess the first and most obvious thing about this book is that it’s not written by me, which is an enormous relief to me in a way because it rather than me bringing all my prejudices and biases and ways of looking at the world, which I brought to the previous books I wrote. This book is written by representatives of our OMS community who bring all their prejudices and biases, and ways of looking at the world which fabulous for me to see. Because after what seems like quite a long time of bringing this message to people and hearing the message coming back to me through the filter of all of these different people’s lives and experiences and joys and sorrows. And it’s just a wonderful read for me to sit down and say that all this has been happening at it in our community and that people have worked out ways of adopting and maintaining this program, many of which I’ve really never considered given that I’ve got only my own particular view of the world. The co-editors in this book, I need to point out are Associate Professor Sandra Neate, who has all sorts of interesting background. But what qualifies her to be a co-editor in particular was that she has facilitated retreats with me for a long time and really has been for those of you who don’t know an incredibly important part of my personal journey and MS. Because Sandra and I are married. And perhaps we can do another webinar sometime on that particular journey. But the other co-editor is Associate Professor Michelle O’Donoghue, who’s from Harvard University and is a cardiologist over there. And I met her in Boston when she came to see a talk that we did there and she’s now been on the program over 10 years and is really a highly regarded cardiologist in her own right and researcher, world class researcher who brings a very particular and very incisive intellect to this editing process for all these contributors. How this really differs from what is in previous books and what’s on the website. What you can get by keeping up with things as they come up on the website is twofold I think, firstly, it reflects our community, the voices of our community, in their sort of take on the science and on the way the program can be adopted and can be maintained in our lives. But importantly, it also brings a really incredible personal voice to it. Every one of those contributors talks in some way very personally About MS. Its effect on the lives. And I think in the book, there are only four contributors who haven’t got MS who are who aren’t on the OMS program, or in fact, some of them are on the OMS program, but don’t have MS. But all the rest are on the program and have MS. And in many ways representative of our community and you can find some personal stories on our website, you can find some in the recovery from MS book, you can find a little of that flavor in mind books. But for me, this is a rich distillation of that sort of wisdom that people get through the lived experience of MS and the Overcoming MS program. So that’s it. From me as an introduction. I think, Johnny and Phil have a couple of questions for me.
Dr. Jonathan White 06:04
Absolutely George I relish the opportunity to ask you a question. Since since your diagnosis 20 years ago, there’s been many, many changes in the MS landscape. I suppose, in the field of MS research generally, how do you feel the OMS program fits into that now 20 years later?
George Jelinek 06:26
Well, I guess it’s fair to say 1999, when I really came up with the OMS program, it’s obviously changed a bit since then. Much of what was said in that very first book in 1999, called Taking Control of Multiple Sclerosis was considered more than revolutionary, it was actually considered crazy. There were many people who thought that this was a wacky idea that lifestyle factors could somehow influence this, this disease that really until that point in history had seemed to sort of run a particular course, for no particular reason. That from one individual to another, there was a wide variability in how that course manifested. But the generally accepted wisdom was there was nothing you could do about that. And really, until the advent of the disease modifying drugs in about ’96-’97, depending on where you lived in the world, they were just coming onto the stage at that point in time. And there’s quite a bit of debate really, about whether they actually even affected the course of MS. They were considered really to modify the number of relapses a person with the relapsing remitting form might get really have no measurable effect on progressive MS. And it was really the prevailing wisdom that there was nothing much you could do. Now what I think the biggest change in the landscape has been is that that’s no longer true. And it’s widely accepted. Now that lifestyle makes a big difference. And this is right across the MS community across our therapeutic community, that clinicians in the area, there’ll be a greater or lesser buy in to the extent that lifestyle makes a difference across that, particularly that clinical community, but there’s no question that it does. And for me, that’s a really big change in the landscape. And people may still debate the role of diet and how effective that is and what degree there has an influence compared to say vitamin D or sunlight or stress or stress relieving techniques, or exercise, but no one would seriously offer the opinion that lifestyle doesn’t make a difference to the course of MS. Or that there’s nothing you can do about the course that is now an accepted part of the landscape in MS. I think Jonny
Dr. Jonathan White 09:17
I couldn’t agree more.
Phil Startin 09:20
Now, Thank you, George. Yeah, I think it’s maybe testament to the research you did 20 years ago, George that now OMS almost seems like it’s mainstream. It is, I mean, in terms of making making those lifestyle interventions, it’s just been much more widely accepted now. But do you think that any modifications needs to be made to the program, do you foresee any new pillars being added or any take taken away?
George Jelinik
Well, one of the things about research and the fact that this is a research and evidence based program is that research is constantly being done. It’s constantly coming in, and any scientist worth his or her salt A watches the research and modifies their opinion and views about whatever disease based on the newest research and the OMS program’s not been any different. I mean, people probably forget those who’ve been around a long time who’ve been on the program a long time might remember that. In 1999, I was advocating a low fat dairy diet with fish oil. There are a number of thing, cod liver oil, in fact, I was recommending vitamin D. Because, of course, we didn’t really have access to the kind of knowledge that we have. Now, it was really only after the first book came out. Within a few short years, we had great work from the Max Planck Institute in in Europe and Toronto, the Hospital for Sick Children doing that really basic work on dairy protein, not the fat in dairy, but the protein. And the way that it could create lesions in the brain of experimental animals when injected into into those animals, just the protein from dairy. So I mean, that was one of the very early changes that dairy was omitted from the program. And really, the program continues to evolve with the drop of fish oil more recently, when HOLISM, for example, found that flaxseed oil was associated with a very significant drop in relapse rates, but fish oil had no discernible relationship with relapse rates or disability. So I think in answer to your question, Phil, I think there’s almost certainly going to be further changes. I mean, if I was to predict where the any new pillars might come from, I think I would probably say, the most promising things would be in the areas of intermittent fasting. Possibly cryotherapy, cold therapy. But also, I think there’s going to be an increasing focus on something that then in our OMS community we take for granted, and that is the enormously beneficial effect of community of social interaction. The things that have always been an integral part of the OMS program, I think research is going to start confirming that that actually contributes significantly to one’s health after a diagnosis of MS.
Phil Startin
Yeah, no, I completely agree. And I think it’s almost one of the understated pillars of OMS is the community pillar. That’s that’s just underpins everything. No, I completely agree. No, thank you. And just another quick question, then in terms of does the book and handbook at all differentiate between the different forms of MS relapsing remitting or secondary progressive or primary progressive in sort of terms of different levels of physical disability or as part of part of the roadmap?
George Jelinek
And for the audience, I didn’t put Phil up to that question, because he wrote the progressive MS chapter. Of course, it’s actually one of the really important things about our OMS community that we are well aware of the significant proportion of our community for whom progressive MS is a significant issue, and for whom disability is a significant issue. And the book tackles that in in different ways. In your chapter particularly well, Phil, in fact, I think, perhaps later on we’ll talk about just how much value I got from reading your chapter. I think it’s an absolutely outstanding chapter in the book on progressive MS and opens up ways of looking at that particular problem that I don’t think have been discussed really anywhere in the medical literature before, not that I’ve seen. And the book really in all the other chapters, there is consideration of that spectrum of disease, type and activity throughout our community. So I think, to some extent, I think the earlier books that I wrote, were a little more focused on what one can do earlier in the course of the illness, probably reflecting my background in that I discovered this within weeks of getting diagnosed. And so I had that very particular mindset of approaching it with the hope of preventing things happening and rather than facing In a situation where you’ve already sustained significant nervous system damage, have significant disability, and are looking for ways of recovering some function from that. So, yes, I think the book is is really particularly relevant.
Phil Startin 13:51
Thank you, George. Thank you.
George Jelinek 15:15
Yeah. Thanks, Phil. And Jonny, I think, time for you to do your introductions isn’t?
Dr. Jonathan White 15:29
Yes, unike you, George, I do need to introduce myself. So for those for those who don’t know me, excuse me, I’m Jonny White. I’m a obstetrician and gynecologist. I’m based in the UK, I live in the north coast of Northern Ireland. And my day job involves early pregnancy care and recurrent pregnancy loss. But I also work for the OMS charity as an event facilitator and a medical advisor. And just to be clear, I was diagnosed with MS in October 2015. And I’ve been following the OMS program since about three days later, and I’ve haven’t stopped since. So I suppose I didn’t edit the book, thank goodness, I was very honored and privileged to be asked to write the medication chapter of the latest book. And I suppose to summarize what it’s about it’s fairly obvious from the title that it is to do with medication, but it’s specifically the disease modifying drugs, a bit of their history, where they’ve come from, where we are now and those that are available. And also, I suppose, the drugs that may come through in the next few years, hopefully, with regards to treatments for progressive forms of MS, and also myelin repair and potentially reversal of nervous system damage. And more than that, though, when I actually think this was possibly the most rewarding part of writing that chapter was, it forced me to think about clinicians and doctors thoughts, feelings about medication, their role and how that interacts with their patients in front of them. And I’m sure many of you will be able to empathize with the idea that for those that say, “Hold on, I need to think about these medications, whether I want to take them or not.” And of course, to be clear, OMS always advocates these medication when required, and if it’s the right decision for you, but that’s the point that you should be given the time and the space and the relevant impartial information to be able to make that decision for yourself. But I also felt was really important to try and explain it from from the doctor’s perspective that imagine how difficult it would have been for them watching people with almost inevitable decline in the early years of treating MS. And and then when medications came around that potentially could change that, although they didn’t know at the time. It must have been very difficult for them to encounter somebody who said, “You know what, there’s more to this than just taking medication.” So I hope that my chapter in some way helps to explain that for you and to lay out the landscape. Of course, you can’t future proof medication. I know the book is designed to be future proof. Unfortunately, that landscape changes so rapidly that it almost needs updated daily at the minute. But it does include resources that you you should check regularly if you if you do have to make decisions about medication.
George Jelinek 18:12
Yeah, thanks for that. I think this whole question about use of DMTs. And having that complement the lifestyle choices is such an important one. And things sometimes discuss quite favorably within the different circles and the Facebook groups. Can you say any any more about how those two sit together and how they can best fit together?
Dr. Jonathan White 18:31
I think sometimes the medical community thinks it’s “us or them” lifestyle or medication. And that could never be further from the truth. I think that, you know, certainly I personally have always chosen to use medication as part of my way of of managing MS. And I wouldn’t change that. But nor would I change using lifestyle to manage my MS because, you know, you’re using a fairly, although it may feel very clever drug but they’re all to a greater or lesser extent, a blunderbuss approach to altering your immune system. And that’s fantastic. And undoubtedly for many people has many benefits and is a huge part of your armor and protecting against this disease. But why ignore the underlying things that caused the problem in the first place, you know, stress, lack of exercise, low vitamin D levels, poor diet and processed and altered fats and animal fats in your diet. But that makes no sense to me that you would do whatever it takes to remain well to be healthy physically and mentally. Why would you take a pill and ignore the rest of it? And I know I’m being flippant about that, but that is part of society, I think wider and more generally a moment that it’s almost like when you take a pill and that fixes a problem. And unfortunately, I’m here to tell you that it doesn’t but coin is that if I didn’t have MS tomorrow, and that’s unlikely to happen. I would certainly still follow OMS tomorrow. I wouldn’t give it up for all green tea in China.
George Jelinek 19:55
Yeah. But it becomes a lifestyle choice, doesn’t it rather than something you’ve got to do
Dr. Jonathan White 19:59
Absolutely. Yeah. So I think unless you want to ask me anything else, you get to talk about yourself.
George Jelinek 20:09
Great. Thanks. I’ll take the chair the rest of the session. So just really, really quick about that. Thank you, Johnny. I’ll just give a really brief a brief introduction myself. So good morning. Good evening. Good afternoon, everyone out there, wherever you are.
Phil Startin
So I’m Phil Startin, I’ve, similarly, I think, pretty much like everyone on the call today, but I’ve got MS. I’ve got Primary Progressive MS. I was diagnosed back in 2007. It took me a few years actually to find OMS. Unlike Jonny, who went straight into OMS, I’m saying I’d probably progressive, I started with no relapses, bit of numbness in my right side of the body, and nothing else. So I think I do what a number of his do, ignored it for a couple of years, then tried a number of different protocols that are out there, before finally stumbling on OMS, back in about 2010-2011. And I followed it. So I thought was pretty pretty good for a couple of years, then fortunately, went on the first non-Australian New Zealand retreat. So that was held in Launde Abbey in the UK, back in 2013. And that was great. And that was really quite a revelation. So it’s where I first met George. And I kind of realized that what I thought I was pretty compliant with OMS. I wasn’t. So I made some really big changes, and I pretty much been 100% following the program, since then, I’m really, really quite compliant with it. Meanwhile, my diet choices have changed a little bit over time. But I’m still following it. But I think I may be just making some better choices now. So my chapter’s about progressive MS. What is it? How’s it different? And how do the different pillars apply to progressive MS? And are there any adjustments you need to make on to it? Perhaps a little bit like Jonny and I think everyone who has asked her to write a chapter for the book. I mean, it was an amazing honor to be asked. So thank you. Thank you. Thank you, George for doing that. And I still really vividly remember that the conversation, the Zoom session I had with George and Sandra, when they talked about the book and asked me to do my chapter. And it was fantastic. And yeah, when a little bit of an effort took to write the book, to be quite honest, I think I got the structure quite quickly, but then filling it all out and writing the chapter and refining it and editing it was it was just a nightmare. So yeah, me in fact, you, George, you’ve done this a few times. I don’t know how you’ve done it. But yes, I can imagine being an editor is much, much easier life than actually sitting down actually writing the thing from start to finish. But it was good if it’s slightly cathartic exercise to do. And I guess the main points that I only wanted to bring out in my chapter was that, even with progressive MS, you can make a difference. So by following the OMS program, you absolutely can make a difference, you can change the trajectory of that condition, you can improve your quality of life. And through neuroplasticity, you can even recover some function. So this this approach is OMS approach and OMS program is just as relevant for us with progressive form the condition. As it is for those with those newly diagnosed and with a relapsing form, possibly even more. So. I think one of the reasons I’m really passionate about this particular point is that I still remember again, very clearly going on the retreat with George back in 2013. And with George and Sandra, and Lynn and Craig, and it was amazing really like life changing week. It’s something that some fantastic people, some of whom are now really, really close friends. But I got to the end of it. I thought that was amazing. But is it gonna work? Because all the research was presented, but much of the research that was talked about, or related to reducing the relapse relapse rates, and I’ve never had a relapse. So what was it wasn’t gonna work for me. But I’ve now been following OMS for about about a decade, I can say absolutely, yes, it does make a difference. And I’ve seen other people with progressive MS following the approach as well. And yes, it does make a difference. So to me, that’s the key point I really wanted it to come across in my chapter that it does make a difference. If you’ve got progressive MS. There may be some some nuances certainly around the exercise, which I actually think from a user perspective is almost the most vital pillar. I think it’s the one in which you get the biggest bang for your buck. So doing a bit of exercise to really make it make a big, big difference. Similarly, mindfulness and how we deal with this condition and the fact it is a degenerative progressive condition can be really hard. And for me you having the OMS to follow is almost as much a mind game, as it is anything else. So dealing with that, and having the tools to deal with that, that mindfulness can can give is fantastic. But yeah, no, it was it was a wonderful process. So amazing to be here with you two gentlemen this morning. One of the things in your chapter, Phil, that really hit me, in addition to what you’ve said, was the way you reflected on how progressive MS can affect your identity. And your advice to sort of ask our audience with progressive MS to, and indeed really all forms of MS to take a step back and reflect perhaps on who they are, and what’s important to them. And I know it’s a very personal thing to be revealing to 600 plus people, perhaps, but what did you learn about yourself through through that process? I’m not quite sure I’m brave enough to go into that drawer. And I know you talk a little bit about about this, you wrote a section chapter in the book. Yeah, and it was quite a hard exercise. And I think the, I guess one of the hallmarks or characteristics of the progressive form is loss of function. And I’ve certainly lost loss of function over the years, both physical and cognitive. And it’s for some changes, so I can no longer do that job I used to do do as a management consultant, I can’t mountain in that was was a love of mine. So and I think we are so often defined, we define ourselves by jobs, by roles in society, but by our hobbies. And when those those change, it really forces you to challenge your identity. So maybe some of the insights that I got is just to just to hold that feeling of identity less tightly, just trying to be open with what’s there to get, maybe just take things a little less seriously. Not hold on to that, that that projection of who I am, in terms of sense in terms of in terms of sort of jobs and roles in society, just do it, do it do it little bit differently. And I’m, again, I’m completely convinced that you can live really well and happily through death through doing that. And it does does make make a huge difference. So yeah, just holding on to life less and holding on to that that concept of I and self a little less tightly. George makes sense. It can make a huge difference. We don’t need to do it. And it gets easier. The more we meditate, really, doesn’t it?
Phil Startin 27:32
It does it that’s it can be a tremendous tool to help. Absolutely.
George Jelinek 27:38
The audience may be unaware that we have a Living Well with progressive MS Circle now, which has about 25 members. How’s that going? Yeah, no, it’s good. It’s going really well. So it was formed a few months ago, now. a chap called Pat Feller is the ambassador. So He’s based in San Diego in the US. I think it’s the first and possibly the only OMS circle that’s not geographically based. So I’m also a member of the West of Scotland circle. And it’s fantastic to meet people locally and face to face now and again, but it’s also nice having this progressive MS circle, and we meet virtually every month or so, I just have chats about the issues facing us as people with some some loss of function. So we might talk about science a little bit or have a have a bitch about our bowel and bladder problems. But that’s just nice to do it in that group. So it’s a no, it’s working really well.
Dr. Jonathan White 28:34
I have to confess that if I had to pick one chapter, and I truly believe it’s Phil’s, for me, that is a paradigm shift. huge, hugely important way of discussing progressive forms of MS that I don’t believe has ever been done. Certainly not as succinctly and as eloquently as Phil does it. Again, this makes me feel physically ill actually saying that. Yeah. Well, thanks. I truly believe that was a sensational piece of work that will stand out on soon right. Rachael Hunter’s chapter as well pains me as slightly but not as much as Phil to say that I in medical circles, it’s not very in vogue to talk about resilience, resilience training for staff, and actually, it really focuses on essentially “toughen up so you can survive how crap it is to work in a health service” a bit better. And actually, that’s completely wrong. And that really, I really struggle with that. But Rachael’s chapter on resilience and harnessing resilience comes at it from a completely different way. There’s actually practical and meaningful and helpful and I love her three P’s. So I am definitely holding on to that one. And my final one is I’m not going to take them any more time. I love Rebecca Hoover saying about having an MS mentor. She meant in the workplace, but I actually love that. You know, I’m very fortunate to have lots and lots of MS mentors in my life, but I think that’s a great idea as well. So I love that and there’s just there’s so many little cookie crumbs you can pick up from the chapters that just, you know, it’s just fantastic. I learned so much. And it was like I was sitting down with OMS friends again, which I’ve really missed in the last two years that we haven’t physically been able to, to get together to meet up to do the work we normally do, but also spend time in our community. And it felt like they were talking to me through this book, and it was, I loved every second of it.
George Jelinek 30:22
Yeah, look, I was blown away, I asked the chapters came in, you can imagine I mean, Sandra, and I really brainstormed this book. And to try and work out how to do something that would really not be just a follow on from the OMS book that I’ve written before. Something that would break new ground, something that would be sort of future proofed, if you like, that didn’t depend on the latest research article or whatever, something that was much more reflective of people’s experiences. And we thought, well, the idea is to get other people to write the book, and to harness their wisdom and their experience, and to distill that right down. And so, I mean, it was taking a bit of a punt in a sense, I knew a lot of these people very well, through retreats, and through other events I’ve done and one or two of them, I actually hadn’t met but were referred to me from people I didn’t know that had great stories that needed tell him. But it was a joy for a couple of years, every week or two or three, I’d open my inbox. And there’d be another chapter that rolled in or another person’s story. And I would sit and read them and and each one just sort of took blinkers away from me about the way I’d looked at the program, the way I looked at adopting this and of course, I’m, I’ve got my own particular foibles and biases. And you know, I can adopt things, you know, wholeheartedly and jump in, and I can do the kind of, you know, the whatever it takes approach that a lot of people have very different approaches than that. And I look, for instance, I mean, I loved Phil’s chapter. Phil’s chapter is gold. It’s a groundbreaking chapter that people are going to talk about into the future with progressive MS. But, you know, there are many others actually, that also made me stop and thinking technologies chapter when that came in. When he described and everyone was really good, I thought in adhering to the kind of metaphor that we wanted to use that roadmap metaphor, the journey that talks about the process, not the outcome, not where we’re headed, but how we get there, you know, that was the whole nature of the book. And Jack had this lovely metaphor of the four lanes on the highway, and there’s the kind of guardrails on both sides with as far as the diet goes, and you never sort of go outside the guardrails, obviously, otherwise you fly off and run into all sorts of trouble. But you can move between lanes, you can choose a lane, for instance, that’s plant based whole food, no oil, no gluten, if you wish, that that’s perfectly in keeping with the OMS diet, but it’s a particular variation that some people will choose, others will choose to do it the sort of more standard way others will choose to have the oils, but you know, not have the seafood and so on. And just to, to see the flexibility of that approach. But a lot of people look at what we present in the OMS program in the way of data and they think, well, that’s really hard. I don’t think I can do it. But when it’s presented in a way where you’ve got a lot of choices and a lot of options. And they’re all perfectly in keeping with that goal of doing the best you can nutritionally for your health. And I think that’s that was a brilliant chapter. But like Johnny, I loved Rachael’s I loved. You know, Sandra, of course, and my daughter, Pia wrote the chapter on families and partners and that’s a very personal chapter to me, but I reflect back and I think, before OMS came along, people were not at all talking about what you might do for the rest of the family, to prevent them developing MS. Or to consider how your particular journey might affect their journey through life and and who we are as a community discussing that openly. And the the difficulties in the stresses are they’re missing one member on the rest of the family and, and the ways that the family can accommodate that and actually make it a joy rather than rather than a chore. And so I mean, there’s many, many examples of that through the book. And of course, the personal stories to me to add this incredible flavor. And each one of them is, there was an attempt at least to chain them into the content of the chapter. So I illustrated that in some ways. So I was very carefully handpick stories of people that I knew, had experienced that program or MS in a way that related to that chapter. So for me to see it all sort of gel together into a final book that is satisfying to read. For me, who, in theory, you know, I’ve been doing this for so long, and I’ve read so much to find out a revelation, I think says a lot to me about the quality of the the contributions that came into that.
Phil Startin 35:58
Certainly, Jack’s chapter on food and again, the swim lanes or the different lanes for the for the choices of food because I think you’re right, George that sometimes their diet can feel quite restrictive, but the way that Jack portrayed it and being very flexible, that having having the boundaries was perfect. I really liked that I thought that was that was a very kind chapter that allowed us just be a bit more kind with ourselves when when following the diet. And I also rate Dr. Rachel Hunter’s chapter. And again, I think this this resilience when you are if you’re function, if you’re losing physical or cognitive function progressively having that resilience that is almost more important. Particularly if you’re kind of used to living with new norms almost constantly, or every month or every few months, that resilience becomes key. So I agree with Johnny, the three P’s approach that Rachael brought out it was excellent. And the little short stories, so just everyone’s contributions, I mean, I’m I’ve got a copy of the book in the toilets. And it’s just great to sit down and just browse. And it’s a lovely book just for dipping in and out of you do not need to read it to cover to cover. It’s just lots of little things in there. It’s delightful. Yeah, really great. Thanks, George, thank you for putting putting it together. It’s perfect.
George Jelinek 37:18
For who don’t know, Sandra, runs the neuro epidemiology unit. And it’s a relatively small unit, but certainly punching well above its weight, in terms of the kind of output we’re seeing from it. I mean, currently, this somewhere around 44 papers that have come out of the HOLISM study alone, in the major neurology journals and public health journals in the world. There’s a wealth of research that’s coming out all the time from the unit. And probably the the slight shifts that have taken place since I left, which is a couple of years ago, have been a reflection of Sandra’s influence on the unit, bringing a much more qualitative life experience sort of focus to the work rather than the quantitative nature of the work that I tended to favor, you know, looking at the proportion of people who, who improved, you know, with with a higher quality diet and that kind of thing, which was always interesting to me, but Sandra’s much more. Now, publishing in the in the area, sort of the experience of people on the program, the experience of people with their traits, the experience of people undertaking mindfulness interventions. Probably the big bit of research that we’re about to seriously embark on is now our new one online course, for OMS. So the OMS online course, is going to be tested in a randomized controlled trial. So we’ve had a PhD student Will Bevan’s just shortly to submit his PhD on the development of that course. And it’s a very rigorously developed course over four years. With really high level input with peer input from people with MS focus groups with the highest level sort of digital health input, in terms of educational principles, and so on, it’s a really good course but the thing people may not know is that we’ve also alongside made a control course. So in medicine, the best proof is when you randomly allocate people to an intervention treatment, a new treatment or standard treatment and see if there’s any benefit from the new treatment. While we’ve also developed a course that reflects current thinking in MS built along the same lines and we’ve done a feasibility randomized controlled trial of that. And it has shown some really interesting stuff which we’re currently publishing. But essentially, we’ve refined the both courses a little on the basis of the feedback we’ve got in the feasibility study. And we’re just about ready to roll it out to the MS community worldwide. In the form of randomized control trials, the difficulty for people with OMS, on the OMS program, and in this community, of course, is that if you join that trial, you may be randomized to the standard care, because it’s an entirely random thing. And you may not wish to do that. So what we’re hoping really is that we get a lot of people who have no exposure to OMS, who sign up and who either are randomly allocated to learning all about how OMS the program works, and how to adopt it. And all of those things, and what the sort of main MS organizations are currently recommending, in the way of drugs and lifestyle, and so on, which obviously is still somewhat different, the two have been sort of gradually approaching each other, but there’s still a gap between. You know, like all scientists, we don’t go in with preconceived notions about which is going to be better, or how much better or anything like that, we’re going to find out when the numbers come in. And I would hope that we get many 1000s of people who randomly are allocated to one of the two, we follow them for a number of years, look at what happens to them their lives to the progression of their MS and so on. For me, that’s going to be a really fascinating study,
Dr. Jonathan White 41:49
As we know, with average bit of research takes 15 years to get to the clinical paradigm. So what I can say is that the relationship between HCPs healthcare professionals and the whole lifestyle field generally, is coming closer together rapidly. And I’ve really felt that accelerate in the last couple of years. And actually COVID has done some favors in that regard. Because certainly within the NHS in the UK, we’re really seeing that health care providers are desperate for people to provide preventative medicine advice, trying to prevent disease, as our population gets sicker, as it lives longer in many cases, and the OMS program is absolutely perfect for that. So hopefully, in time, it will simply be that you don’t need OMS to get that message because it will just be accepted as mainstream wisdom is that that is the holy grail. It’s a bit of a watch this space. But I’m very, very optimistic. I honestly started in the last two years, I felt that that changed the way I was invited to speak at the MS Academy last month, which was probably unheard of two years ago. And I wanted to give my thoughts about diet and lifestyle and MS. And for UK neurologists follow me up and say I’m not going to disagree with the single thing you’ve said was, I think a fairly big, big sea change going the right way.
George Jelinek 43:01
Look, I think it’s important for people to be aware that fatigue, I mean, everyone I think in the MS community knows that fatigue is a really, really common symptom. It’s the most common symptom that people get, and in various different studies around you know, the 80% mark, a lot of people get fatigue, once they’ve been diagnosed with MS. One of the one of the really important things about the program seems to it seems to significantly affect fatigue. And the HOLISM work supports that it shows that people you know, the more people follow these healthy lifestyle behaviors, the less fatigue they have. There are many studies now starting to sort of show similar things. So, for instance, a study some years ago, on a whole food plant based diet randomized control trial, showed that the whole food plant based plant based diet, significantly reduced fatigue in the treated population versus the control population. We know that following the program is probably the best single way that people can address the issue of fatigue. Of course, that doesn’t mean it’ll go away for everyone who follows the program. It the program is about reducing risk, the risk of fatigue is reduced if you follow the program, and better your follow up the more it’s reduced. But for many people are still have it. So what other things are there that people can do what well one of the well studied aspects of the program is exercise as a treatment for fatigue, and this sort of seems paradoxical, of course, because if you are fatigued and you’re really really struggling to even get off the couch, the last thing you really consider is exercise. And yet, paradoxically, that is the thing that’s going to make you most likely if you can commit to it on some sort of regular basis, most likely to actually see that symptom diminishing and reducing, it’s significant. So I have to say that all of those lifestyle factors, and exercise in particular, certainly work better than anything that’s been tried in the pharmaceutical world. So the pharmaceuticals in general have been uniformly unhelpful for fatigue, and I’ve tried many Amantadine, Modafinil, that isn’t to say that the occasional person won’t get benefit from them. But where they’ve been studied in a big group of people who’ve taken say Modafinil, compared to a big group of people who’ve had placebo, there’s been no difference in the rates of fatigue within those groups in in meta analyses. So I think for this audience, it’s important not to pin your hopes on medications doing it, but rather, like with many aspects of MS. Coming to a realization that much of this, the best control you will have will be in your own hands. And the things you can do for yourself, are more important than what any outside agency can do for you. With regard to fatigue.
Phil Startin 46:33
George, maybe just to speak on a few points you raise, I completely agree. I think exercise is really key. I know, it helps me, I think there’s a nice phrase, which is if you’re feeling really, really tired and exhausted, that actually sometimes exercise may make a difference. So when you leave when you’re feeling great and upbeat, actually, your motivation precedes activity. But if you are feeling really fatigued, actually, it’s the other way around. Exercise precedes motivation. So it’s amazing if you do some exercise, how much better you feel afterwards. And it can do really take away some sort of those those feelings of fatigue. But interestingly, in the UK, the National Institute for Clinical Excellence, it’s a kind of a drug commissioning body in the UK, has recommends mindfulness for MS for one area. And that’s in the treatment of fatigue, which I think is really, really interesting, but there is some research that substantiates that as well. So also, just a tip is just to be just to be kind with yourself to I mean, if you are exhausted, then yeah, take a break and respect that. So it’s so it I mean, again, there’s so many expectations society that we should be up and busy all the time. But fatigue is real. And if you need to take a sleep, then then take a sleep if you can, it’s there’s nothing wrong in doing that at all.
George Jelinek 47:50
Yeah, and I have to second the mindfulness part for all because just personally and I generally speak from sort of research experience, but my personal experiences. When I was getting a lot of fatigue, mindfulness was the single biggest thing that helped me. And I often feel you know, this as I tend not to relate fatigue to MS so much. When I feel fatigued, I just see it as feeling fatigue, without particular reference to any illness because for MS, I’ve sort of moved it out of a central role in my life. So I don’t tend to relate things to it. But what I find when I feel like that, and I meditate is that it always feels, I started to feel like I’m almost slugging into some more universal form of energy. That somehow recharges me it doesn’t matter what the cause of that tiredness or fatigue on a particular day is. After I’ve meditated, I always feel like I’ve just had my batteries topped up. I don’t know how much of any common experience that is for other people and sometimes I’ll I always had at least one today but sometimes I’ll do it twice a day on days when I’m feeling particularly fatigued and I find that you know, really fatigued doesn’t stand a chance after my second meditation
Dr. Jonathan White 49:25
You quite often see this sort of analogy of being an MS warrior or you know fighting and not giving up and actually i i personally have never really liked that. You know, I know George has talked about this in books before but the idea of if you have an autoimmune condition where you’re essentially attacking yourself in simple terms, you don’t want to create yet another fight in your head so to speak. So for me I’ve always tried to sort of really view this as me living with MS and me trying to live very well and I think that I do live very well with MS or my MS. You’re absolutely right, the research does quite clearly show that that positive mindset, that sense of mastery of control is extremely beneficial not only to your mental and physical health, but you know, at an immunological level, it actually physically changes how your immune system responds, you know, turns down inflammation for you to have that sort of positive sense of locus of control to say, you know, this isn’t a war on many fronts. This is me, and I accept that I’m living with it, and I’m doing my best. And I’m going to live well. And yeah, that’s that would be my view on that one.
George Jelinek 50:34
Yeah, I think a lot of it’s about that shift that happens when you when you begin to sort of look at the choices that you have, in response to the illness, and most particularly the shift that happens when you stop the reliance on external agencies and agents to improve your health and, begin to rely on your own internal agency. And the things you can do for yourself, and I think the program works on a whole lot of different levels that clearly works on the physical level. And there’s not much dispute about that. But actually, there’s some really profound benefits around that sense of agency and mastery that one has by taking control and adopting and sort of a position where things aren’t imposed from outside of that their choices that one makes for because you begin to see that the future is actually much more in your hands than in the hands of balance. I think that sort of sense of agency, as Johnny says, kind of plays out in not only your your physical health, but your emotional health, and your mental health. And I think that, that it sounds deceptively simple, adopting a very particular form of diet. But it’s the adoption as much as the diet that changes that mindset and that view of oneself as being in control rather than being controlled by the illness.
Phil Startin 52:29
And I agree with everything that my two colleagues have said. And that’s one of the reasons I really like the fact that mindfulness is part of the program is that it brings a gentleness and kindness to it, that to me just just underpins everything we do as part of part of the OMS program. And just by adopting these these, these new strategies, new, these new elements to the program, you’re being kind to yourself. You could be kind to your own health and well being and sometimes teach mindfulness so that you can actually replace the word mindfulness with the word kindfullness, and treat them quite synonymously. So it’s, I think that that that that that really helps with what we’re trying to do as well. So yeah, it’s really works in such such a profound level for the whole program.
Outro 53:22
Thank you for listening to this episode of living well with MS. Please check out this episode’s show notes at overcomingms.org/podcast you’ll find useful links and bonus information there. Have questions or ideas to share? Email us at podcast at overcomingms.org or you can reach out to Geoff on Twitter @GeoffAllix. We’d love to hear from you. Thanks again for tuning in and see you next time for tips on living a full and happy life with MS.
Subscribe to this podcast and never miss an episode. Listen to our archive of Living Well with MS episodes here. If you like Living Well with MS, please leave a 5-star review.
Feel free to share your comments and suggestions for future guests and episode topics by emailing [email protected].
Make sure you sign up to our newsletter to hear our latest tips and news about living a full and vibrant life with MS.
If you enjoy this podcast and want to support the ongoing work of Overcoming MS, we would really appreciate it if you could leave a donation here. Every donation, however small, helps us to share the podcast with more people on how to live well with MS.
Professor George Jelinek developed the Overcoming MS Program and founded the Neuroepidemiology Unit at the University of Melbourne’s School of Population and Global Health which continues to research its benefits.
When George was diagnosed with MS in 1999, he was determined to do something. His mother had died as a consequence of her MS, which spurred him on to sort through and assess the medical literature on MS. His career as a Professor in Emergency Medicine and his background as Editor-in-Chief of a major medical journal gave him the tools to do this.
It became clear to George that remaining well after a diagnosis of MS is more than just a possibility. He found that with commitment to the right lifestyle changes, there is the real probability that many people with MS can live long, healthy lives, relatively free of the usual problems associated with the illness. These lifestyle recommendations are now referred to as the Overcoming MS Program, which he detailed in his book Overcoming Multiple Sclerosis. The new book in this podcast episode is a newly launched accessible overview of his findings.
George has remained free of further relapses, as have many people who follow the Overcoming MS Program.
Jonathan went to University of Glasgow Medical School, graduating in 2008 (MBChB). He completed a further five years of training in Obstetrics and Gynecology and is a member of the Royal College of Obstetricians & Gynecologists (MRCOG). He works at the Causeway Hospital, Coleraine and has a special interest in early pregnancy and recurrent pregnancy loss.
In April 2022, Jonathan was awarded “Doctor of the Year” at the inaugural Northern Ireland Health and Social Care Awards. He contributed to the new book in this podcast episode.
Jonathan was diagnosed with RRMS in October 2015 and has been following the Overcoming MS Program ever since. Dr. White assists Overcoming MS as a medical advisor and event facilitator.
He lives on the North Coast of Northern Ireland, is married to Jenny and father to Angus and Struan. His interests include the great outdoors, cycling and running (reluctantly), reading, rugby, film and spending time with his family.
After a DPhil in Quantum Physics, Phil left his academic roots for a more peripatetic career in management consulting, initially with Price Waterhouse. After years of travelling around the world for both work and pleasure, including a two-year assignment in Geneva, he was diagnosed with Primary Progressive MS (PPMS) in 2007.
Phil discovered Overcoming MS in 2011, and coupled with his earlier discovery of mindfulness meditation, it awakened a whole new area in his life. With training and supervision from Bangor University, he now teaches an eight-week mindfulness-based stress reduction (MBSR) course to people with MS and to the general community on a pro-bono basis. He is also a trustee for MS-UK.
Phil lives in Arrochar, Scotland with his American wife, Cristina, whom he met over a weekend at the Jazz Fest in New Orleans. Phil’s completely convinced that the Overcoming MS program and mindfulness have positively affected the trajectory of his condition.