Side Effects of Natalizumab
Common side effects at the time of the infusion include dizziness, inflammation of the nose and throat, nausea, vomiting, skin rash, urinary and respiratory tract infections. Tysabri may affect liver function but this generally recovers once treatment is stopped.
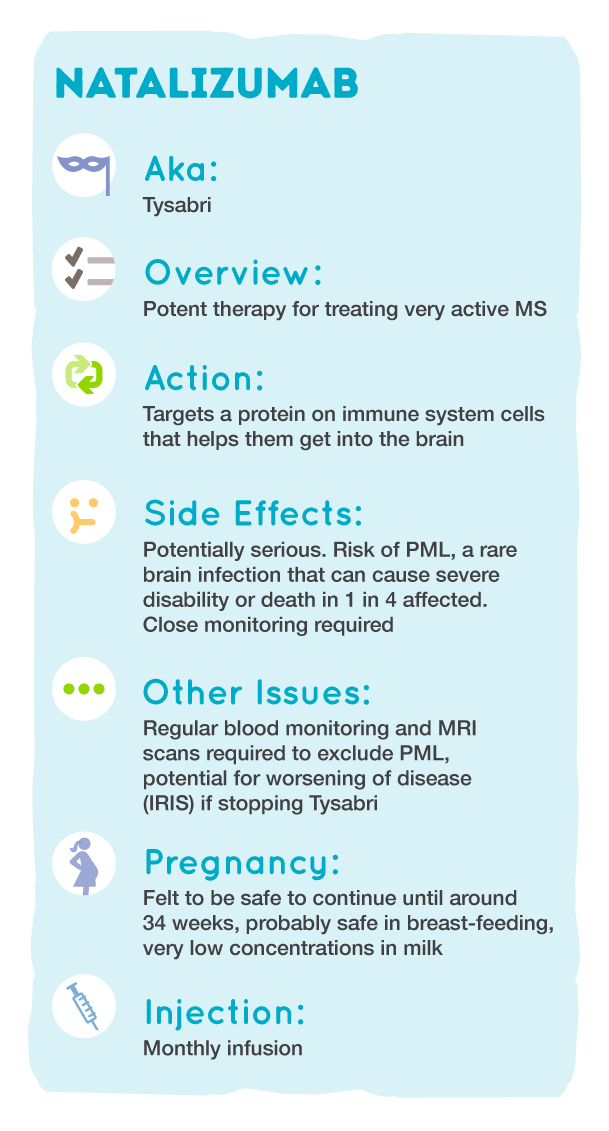
Treatment with Tysabri may increase the risk of developing the uncommon brain infection progressive multifocal leukoencephalopathy (PML). This is caused by the John Cunningham (JC) virus, which is carried by 50-70% of the population, and is usually kept under control by the immune system, causing no problems.
When the immune system is intentionally compromised by Tysabri however, the virus can potentially activate and cause inflammation and damage to the brain. There is currently no treatment, and If someone develops PML, the risk of severe disability or death is 25%.
A blood test can detect the JC virus and give an indication of the risk that you might develop PML. If someone tests negative for JC virus, the risk of PML is approximately 1 in 10,000. If the test is positive, the average risk is 1 in 500, increasing after 2 years of treatment. Another factor which increases the risk of PML is previous treatment with an immunosuppressant drug (e.g azathioprine or methotrexate)
Your neurologist or MS nurse will discuss the JC virus blood test and how it may affect the benefits and risks of treatment.
When you start taking Tysabri you will be informed of the early signs and symptoms of PML. These can be similar to an MS relapse, so it is important to report any new or worsening symptoms. If PML is suspected at any point during treatment, the drug will be discontinued immediately. You will have regular blood tests and MRIs to detect any early changes that may indicate PML.
If treatment with Tysabri is stopped, there is a chance that your MS may become worse than before starting treatment. This is known as rebound or immune reconstitution inflammatory syndrome (IRIS). At present there is much research into which if any of the other MS treatments may be effective in preventing this, with fingolimod and ocrelizumab commonly being used in practice.
Page last updated 29 July 2019